Patient Resources
Patient ID card: A Conformis patient ID card makes travel more convenient* and makes it easier to let others know that you have a Conformis knee implant.
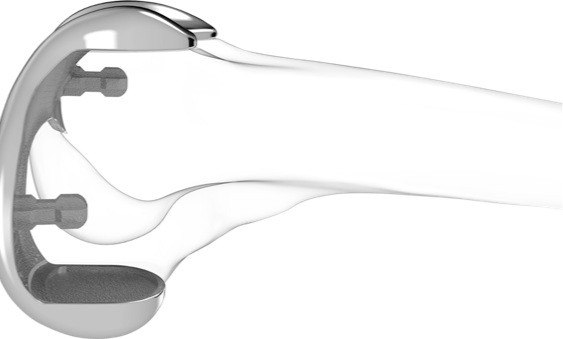
About the knee: We start with a simple idea: make the implant fit the patient rather than force the patient fit the implant
Patient Advocates
Hear from real patients now living with personalized Conformis implants
Patient Advocates